Understanding compliance and integrity in healthcare payments
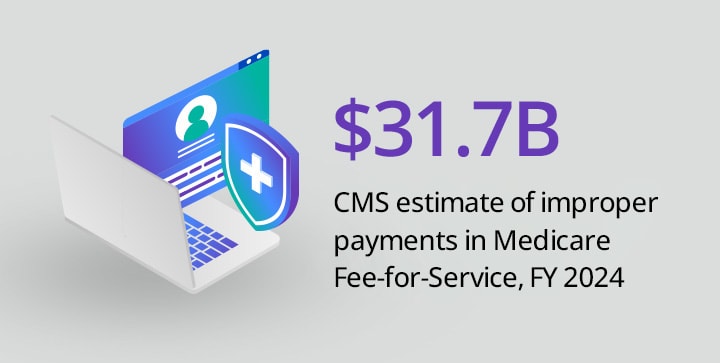
Every year, billions of healthcare dollars are lost to improper payments, errors and fraud. These losses create ongoing financial strain on payers and providers. As regulations tighten, oversight intensifies and claims workflows grow more complex, the margin for error keeps shrinking.
Strong compliance and payment integrity practices not only prevent errors and penalties — they protect revenue, strengthen member and provider relationships and support patient care.
Healthcare organizations that combine clear governance, skilled teams and technology-driven solutions are better positioned to detect fraud early, recover overpayments and maintain confidence in an increasingly scrutinized landscape.
Defining healthcare payment integrity and compliance
Healthcare payment integrity refers to the processes and technologies that ensure payments are accurate, appropriate and compliant with regulatory requirements. It’s about verifying that claims are billed correctly, identifying discrepancies and preventing fraud, waste and abuse before they drain resources.
Compliance focuses on following the rules established by federal and state agencies such as the Centers for Medicare and Medicaid Services (CMS) and the Office of Inspector General (OIG) as well as enforcement initiatives like the False Claims Act and other efforts aimed at Medicare fraud prevention.
Together, compliance and payment integrity form a safeguard against improper billing and a cornerstone of sound financial stewardship.
When these two disciplines align, payers can reduce overpayments, detect systemic weaknesses, stay ahead of evolving regulations and uphold transparent relationships with providers — especially when supported by expert payment integrity solutions.
With CMS and OIG initiatives evolving and new state-level mandates on the horizon, staying ahead means continuous updating of policies, training and technology for health plans to maintain healthcare payment compliance.
The challenges of maintaining payment integrity
Even the most vigilant organizations struggle to maintain airtight payment integrity. Fragmented systems, manual workflows and shifting policies create gaps that can easily lead to missed flags, billing errors or delayed recoveries. Over time, these gaps can add up to significant financial losses, audit risk and reputational damage.
Health plans often contend with:
- Siloed data systems: Payer and provider information frequently exist in separate platforms, making real-time reconciliation difficult.
- Complex coding requirements: As coding rules grow more intricate, even experienced teams are vulnerable to mistakes.
- Limited resources and bandwidth: Smaller or stretched teams can struggle to keep pace with evolving regulations.
- Regulatory complexity: Continuous updates from CMS, OIG and state programs require constant monitoring and adaptation.
These challenges highlight the critical need for smarter, more connected approaches — combining skilled teams, technology-enabled oversight and streamlined workflows and specialized solutions like credit balance services to reduce risk, prevent overpayments and ensure healthcare compliance management across every stage of the payment process.
How technology strengthens claims accuracy and regulatory adherence
New technology advancements are giving payers smarter tools that turn complexity into clarity. Automated claims reviews, predictive analytics and intelligent oversight streamline workflows, detect errors early and reduce the risk of costly overpayments.
Embedding these capabilities into everyday processes helps health plans safeguard revenue, improve operational efficiency and stay ahead of evolving medical regulatory compliance standards, with tools such as coordination of benefits services providing added clarity across claims workflows.
Payers can now leverage advanced platforms and analytics to:
- Automate claims reviews: AI-powered pre- and post-payment checks flag anomalies, prevent errors and accelerate approvals.
- Detect fraud, waste and abuse: Predictive analytics uncover unusual patterns before payments are issued, reducing financial risk and strengthening fraud, waste and abuse detection.
- Integrate compliance checkpoints: Intelligent oversight ensures claims adhere to federal and state policies, minimizing audit exposure.
- Support audits and reporting: Scalable platforms enable continuous monitoring, clear reporting and evidence-ready documentation.
These solutions give compliance officers, billing specialists and IT leaders a real-time view into financial performance and risk. Rather than reacting to issues after the fact, payers can proactively prevent errors, streamline claims workflows and enhance both operational and regulatory outcomes.
Fostering a culture of accuracy and integrity
Technology alone can’t ensure financial accuracy or consistent regulatory alignment for health plans. Those traits critical to operational excellence are reinforced through policy, accountability and collaboration. Leading plans treat payment integrity not as a back-office function but as a strategic imperative driving financial resilience and public trust.
Health plans that invest in people, processes and governance create an environment where compliance and claims accuracy are embedded in day-to-day operations.
Successful payers apply diverse strategies including:
- Investing in staff education and training around coding, regulations monitoring and compliance strategies to build confidence and consistency across teams.
- Conducting regular audits to detect emerging issues, identify trends, correct errors and address systemic issues before they escalate.
- Fostering cross-functional communication among finance, compliance, IT, clinical and operations teams to ensure policies are consistently applied.
- Benchmarking programs against standards such as federal and state regulations, CMS guidance and industry best practices to stay ahead of changing requirements.
- Partnering with an expert solutions provider to access specialized services, supplement internal capabilities and reinforce financial and compliance controls as well as healthcare provider payment integrity.
Leveraging skilled teams, robust automation-fueled processes and intelligent tools, payers can turn compliance from a reactive task into a proactive strategy — reducing risk, protecting revenue and maintaining confidence with regulators, members and providers.
A smarter path forward
Modern payment integrity in healthcare demands more than compliance — it requires a connected ecosystem where people, processes and technology align to keep payments accurate, transparent and compliant. Health plans that achieve this integration can respond faster to regulatory changes, identify discrepancies before they become losses and strengthen member and provider trust across their networks.
Conduent helps payers meet these goals with Healthcare Payment Integrity Solutions that enhance claims accuracy, streamline recoveries and uncover savings opportunities across coordination of benefits, subrogation, credit balance, pharmacy audit and emergency department coding.
Real-world results underscore the impact. Conduent’s subrogation solutions delivered $3B in recoveries for a leading health plan — just one example of the value our integrated payment integrity programs can deliver for healthcare payers.
Together with our broader Healthcare Payer Solutions, Conduent enables health plans to build integrity into every stage of their payment operations.
Frequently asked questions (FAQs)
What is healthcare payment integrity and why is it important?
Healthcare payment integrity ensures claims are accurate, legitimate and reimbursed appropriately. It reduces waste, prevents fraud and maintains transparency across payer and provider systems.
How can healthcare organizations improve medical billing compliance?
Across the healthcare industry, organizations can improve compliance through consistent training, automated audits and integrated technology. Tools that validate claims and flag potential issues before submission help minimize risk and accelerate reimbursement.
What are the biggest risks to payment integrity in healthcare?
Common risks include coding errors, duplicate claims, medically unnecessary services and fraud. Fragmented systems and outdated processes often amplify these vulnerabilities.
How does technology support payment integrity?
Automation, predictive analytics and AI can analyze large volumes of claims data to detect unusual patterns or errors. These technologies enhance accuracy, ensure compliance and reduce administrative burden.
What steps can payers and providers take to proactively protect payments?
Implementing ongoing education programs, automated audits, cross-team collaboration and benchmarking against regulatory standards are practical steps. Partnering with an experienced solutions expert can also provide access to expertise and scalable support.