Simplifying patient billing: How to improve your revenue cycle
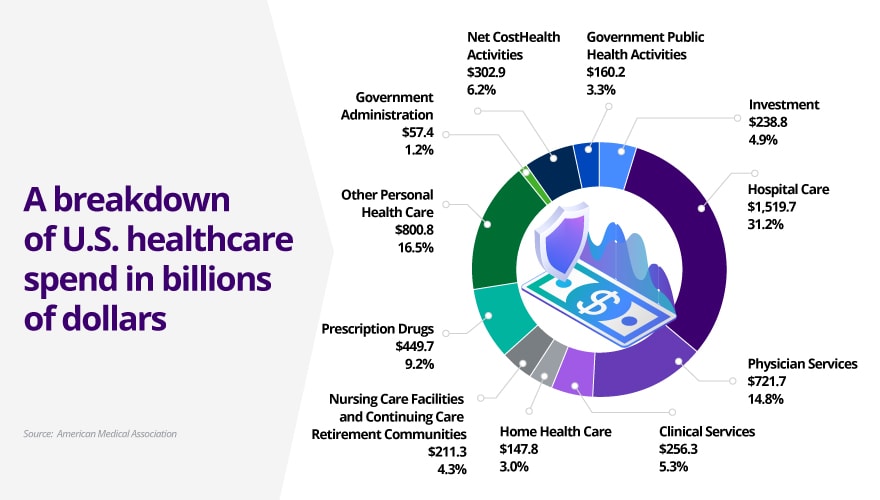
Healthcare costs in the U.S. exceeded $5 trillion last year and they are only going up. With a population that is living longer, rising prices for medical services and pharmaceuticals and the increasing complexity of the healthcare system, 2024 saw an 8.2% increase in healthcare costs. That’s a sharp jump from the 4.6% increase of 2022. And, apart from the 10.4% rise we saw from the COVID pandemic, it’s the highest growth rate seen since 2003, which was 8.5%. But what can be done to taper these skyrocketing costs? The answer may be as simple as looking at your patient billing.
Understanding the healthcare revenue cycle
The healthcare revenue cycle encompasses every step from patient registration to the final payment of a medical bill. This process involves scheduling, insurance verification, service documentation, claims submission, payment processing and collections. Patient billing sits at the center of this cycle. Its efficiency directly impacts revenue flow and patient satisfaction.
As a response to rising out-of-pocket costs, consumer expectations for transparency and the increasing complexity of healthcare billing, modern healthcare revenue cycle management (RCM) is shifting toward more patient-friendly models. The focus is on simplifying the patient financial experience while improving operational efficiency for providers. Patients have come to expect the same clarity and convenience from healthcare billing that they get from retail or banking. This means upfront cost estimates, mobile access and personalized communication. On the other hand, as patient financial responsibility increases (due to high-deductible plans), providers must rethink their billing strategies to reduce bad debt and increase collections — without damaging patient satisfaction.
Common billing challenges facing providers and patients
For healthcare providers, common billing challenges include high rates of claim denials, reliance on outdated billing systems, rising administrative costs and managing multiple, disconnected payment platforms. These issues contribute to delays in revenue collection and increased workload for staff.
Patients face a different set of challenges: vague pricing, complicated bills, limited payment flexibility and increasing out-of-pocket expenses. Many delay or avoid payments due to confusion or financial hardship, which only end up compounding the issue.
To address these concerns, providers must simplify medical billing. This means not just to speeding up collections but also improving the patient financial experience. Clear, user-friendly billing can build trust and encourage timely payments.
The role of technology in modern billing solutions
Technology plays a vital role in modernizing outdated billing systems into patient-centered platforms. Integrated healthcare billing systems that connect with electronic health records (EHRs) enable seamless data flow and reduce redundancy.
Smart tools like chatbots, online portals and AI-powered analytics help patients understand their bills, ask questions and make payments anytime, anywhere. Automation also eliminates manual workflows, reducing human error and speeding up revenue cycle tasks.
Ultimately, medical billing solutions that are digital-first, intelligent, and integrated lay the foundation for a healthier financial future, for both providers and their patients.
Key digital tools and automation transforming billing
Digital tools and automation are transforming traditional billing systems, making them easier to navigate for both providers and patients. Here are some examples of ways digital tools are providing real life impact:
- Automated patient estimates and price transparency tools provide real-time cost estimates before care is delivered, including copays, deductibles, and insurance coverage.
- AI-powered eligibility and benefits verification automate insurance checks to ensure coverage details are accurate before treatment.
- Automated claims management and denial prevention use machine learning to spot and correct errors in claims before submission, reducing denials and delays.
- Digital-first billing replaces mailed, paper bills with mobile-friendly statements via email, text or app. These notifications are interactive and easy to understand, meeting patients where they are.
- Self-service portals are an essential part of enabling digital-first billing as they let patients view, understand and pay bills online, often with flexible payment options and personalized messages.
- Chatbots and virtual financial assistants answer common billing questions, help patients apply for financial aid, and guide them through the payment process.
With these tools, providers are experiencing faster collections and reduced accounts receivable (AR) days, improving cash flow and operational efficiency. For patients, fewer billing surprises and greater clarity have resulted in improved satisfaction. The overall financial process has become more transparent, building greater trust between providers and patients. Additionally, personalized, omnichannel communication strategies are driving higher patient engagement and increasing the likelihood of on-time payments. Here is an overview of the types of digital tools available:
Strategies to simplify patient billing and improve collections
It’s not enough to just provide digital tools. Simplifying patient billing requires a shift to smarter, more patient-centric practices. Conduent offers a variety of strategies that help healthcare providers improve collections while enhancing patient engagement, such as:
- Transparent estimates: Provide upfront cost estimates and pre-service billing information, helping patients make informed decisions and reducing surprise bills.
- Flexible payment plans: Offer installment options and self-service payment portals that accommodate various financial situations.
- Real-time eligibility checks: Instantly verify insurance coverage to reduce claim errors and prevent unexpected costs for patients.
- Automation and AI: Use intelligent automation to streamline claims follow-up, reduce errors, and personalize patient outreach based on behavior or risk.
These revenue cycle improvement strategies make the process more efficient and reduce administrative workloads, while improving collection rates and patient satisfaction.
How Conduent supports smarter, simpler patient billing
Our Healthcare Business Solutions help organizations optimize revenue cycle operations by combining operational expertise with advanced digital solutions. From registration to final payment, Conduent improves accuracy, reduces friction and enhances the overall patient experience.
Through our Health Plan Administration Services, Conduent offers digital patient payments, real-time eligibility checks, automated workflows and patient engagement strategies that drive collections while reducing administrative burden.
Whether your goal is to streamline back-office processes or enhance front-end engagement, Conduent healthcare brings technology and empathy together to transform patient billing into a more transparent, efficient experience.
What’s next for healthcare billing?
As healthcare costs rise and billing becomes more complex, both patients and providers are feeling the strain. Confusing statements, delayed payments and administrative burdens are common pain points across the industry. Simplifying patient billing can ease these issues by making billing clearer, faster and more efficient.
Simplifying the billing experience isn’t just about speeding up payments, it’s about creating a more transparent, equitable and efficient healthcare system. By modernizing billing practices and leveraging smart digital tools, providers can reduce financial friction and strengthen their bottom line. Visit our blog for more key insights into what’s next for healthcare.
FAQs
What is the healthcare revenue cycle?
The healthcare revenue cycle refers to the financial process healthcare providers use to manage patient services revenue, from registration and insurance verification to billing and final payment.
Why is patient billing so complex?
Patient billing often involves multiple payers, unclear pricing, insurance changes, and outdated systems, making it difficult for patients to understand and for providers to manage.
How can digital tools simplify medical billing?
Digital tools enable real-time eligibility checks, transparent pricing, mobile billing and automated workflows, all of which make billing faster and easier for everyone involved.
What are the benefits of simplifying patient billing?
Simplifying billing improves patient satisfaction, accelerates payments, reduces administrative work and increases overall revenue cycle performance.
What is the role of AI in healthcare revenue cycle management?
AI helps automate claims management, predict patient payment behaviors, reduce denials and personalize communications, all leading to faster, more accurate revenue cycle operations.
How does Conduent help healthcare providers improve patient payments?
Conduent offers integrated billing platforms, digital payment options, flexible plans and AI-powered automation that enhance patient engagement and improve payment outcomes.