A return to state-led Medicaid pharmacy programs
Why agencies are reasserting control toward configurable, state-led operations
Within the machinery of state government, few programs are as complex as the Medicaid pharmacy benefit. Behind the scenes of every prescription is a complicated architecture of systems, contracts, clinical decisions and regulatory compliance that must balance cost control with quality of care.
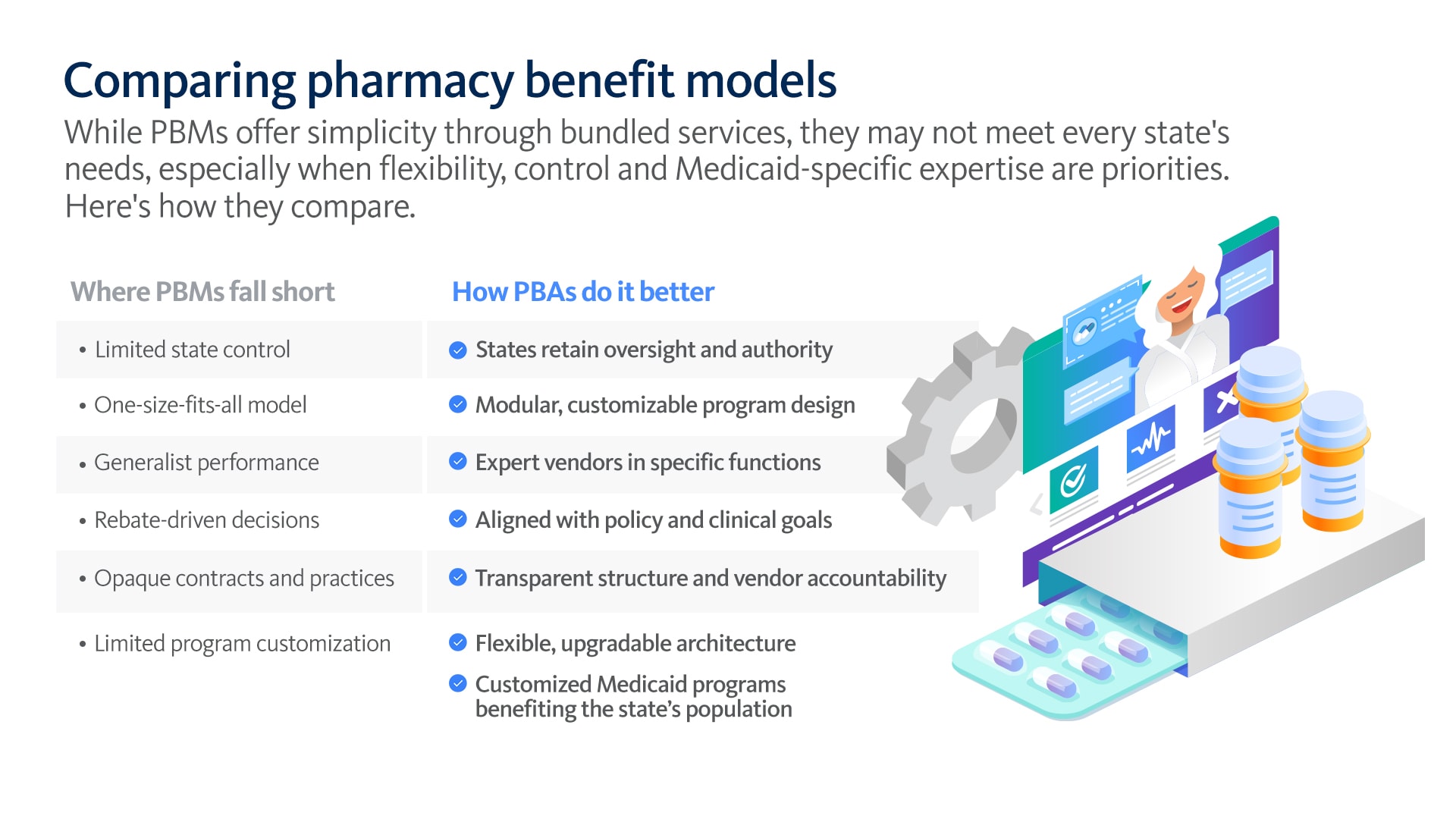
Agencies must walk a fine line between the ease of outsourcing everything to one vendor or the greater precision and accountability that comes from solutions shaped by their own experts. That choice is more than operational. It’s philosophical. And it’s where pharmacy benefit administrators (PBAs) offer a compelling alternative.
A model rooted in flexibility and expertise
Unlike full-service pharmacy benefit managers (PBMs), which package services under one vendor, PBAs allow states to select partners for individual components, including claims processing, rebate operations and clinical support while retaining hands-on oversight of program direction. This modular approach prioritizes customization, agility, and most importantly, subject-matter expertise.
PBA models let program administrators make decisions based on the needs of their populations, rather than relying on national PBM formularies or generalized cost-saving strategies. That distinction is crucial in a program as diverse and politically nuanced as Medicaid.

A shrinking but resilient footprint
The shift toward PBMs has been driven by a desire to streamline administration and reduce administrative overhead. But those gains come at a cost: less flexibility, less transparency and diminished control over clinical decision-making resulting in a generalized program that may not address the state’s Medicaid population and care quality standards.
As commercial PBMs enter the Medicaid space to expand market share, more fee-for-service states are being pulled toward one-size-fits-all solutions modeled after commercial plans. While the efficiencies may be appealing on paper, the unique nature of Medicaid and its populations, regulations and accountability structures often demands a more tailored approach. When states adopt models without the necessary customization, it can lead to gaps in care, reduced transparency and policies that aren’t met or aligned with the needs of vulnerable populations. Over time, this can result in poorer health outcomes, less effective cost management, and diminished public trust in the Medicaid program.
Some states are starting to reassert that control. Several state Medicaid programs are exploring carve-outs and best-in-class vendor models that closely resemble the PBA approach. This allows the state to select the vendor that can best represent their program goals for each of the various PBA specialties, such as pharmacy claims processing and clinical rules, rebates and analytics.
Related: Beyond adversity: A new approach to making Medicare and Medicaid audits beneficial
Conduent’s role in preserving Medicaid integrity
Conduent is among the few organizations still deeply invested in the PBA model. We don’t try to be all things to all programs. Instead, we offer deep expertise in the areas that matter most: high-performance Medicaid-only claims systems, rigorous rebate operations programs along with the personnel and tools that support the state’s Medicaid clinical strategy.
By working alongside state Medicaid staff rather than replacing them, our experts help agencies turn their program goals into achievements through pharmacy clinical rules customized for their distinct Medicaid programs and legislative mandates. We support states in maintaining compliance, maximizing rebate recoveries and ensuring their beneficiaries get the right medications, at the right time, under policies crafted by those who know their residents best. We take these concepts and turn them into actionable realities within the pharmacy program limiting the administrative burden to Medicaid administrators.
A philosophical crossroads
The current environment represents more than a structural shift. It is a defining moment in how states choose to deliver care. The trend toward PBMs is real. But so is the risk of losing the local, expert-driven decision-making that Medicaid administrators require, and the specialty programs to support those populations.
This is not about looking back. It’s about moving forward to optimize programs and member needs.
Don’t settle for generalist models
With the right PBA partner, agencies can regain clarity, flexibility and impact. Conduent is proud to support state programs with tools, strategies and Medicaid-specific expertise. Learn how we can help at Conduent.com.